How to avail of PhilHealth Benefits?
- Updated copy of Member Data Record (MDR). In the case of the dependent being hospitalized, his/her name must be listed in the MDR.
- Original copy of PhilHealth Claim Form 1, available at Philhealth, that has been signed by your employer.
- Receipt of Premium Payments
- PhilHealth ID and Valid ID
How to take advantage of PhilHealth’s benefits?
Your qualified dependents can also take advantage of the abovementioned PhilHealth benefits. Submit the documents to your PhilHealth partner hospital before being discharged so that they can already deduct PhilHealth’s subsidy to your total medical bill.
What are the requirements to avail PhilHealth benefits?
To avail of PhilHealth benefits, you must have at least three months of contribution within the immediate six months before your dependent is confined. Claiming of benefits and its requirements are the same.
How to apply for PhilHealth insurance?
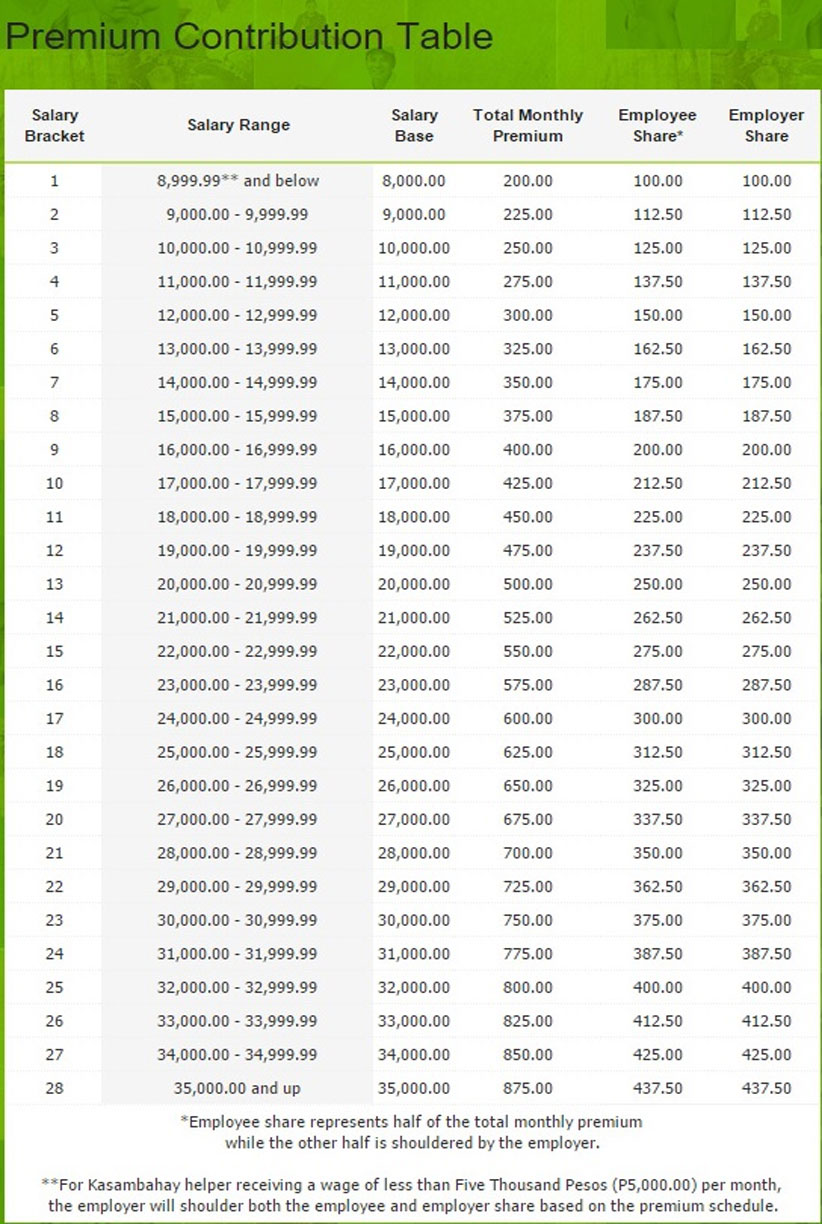
Fill out two copies of PMRF and submit the accomplished forms. Your PhilHealth contribution depends on your monthly salary and your type of employment. Half of your monthly premium is paid by your employer, while the rest is deducted from your salary.
Are you financially prepared for PhilHealth?
A lot of people rely to PhilHealth during the times when they’re confined to the hospital and are not financially prepared for it. A huge part of the hospital bill may be deducted because of the membership and contribution remitted to the agency.

How do I claim PhilHealth benefits?
To avail themselves of the PhilHealth benefits, they should pay at least one (1) month premium contribution within the 3-month shifting period, prior to hospital discharge and must show proof of sufficient regularity of premium contributions.
How can I avail medical assistance from PhilHealth?
To be eligible to avail of your PhilHealth benefits when hospitalized, the following conditions must be met:Payment of at least 3 months' worth of premiums within the immediate 6 months of confinement. ... Confinement in an accredited hospital for 24 hours due to illness or disease requiring hospitalization.More items...
How many contributions should I pay to avail of PhilHealth benefits?
Therefore, to be eligible for PhilHealth benefits, you should have paid a total of at least nine monthly contributions within the 12 months immediately before the first day of confinement. The 12-month period includes the confinement month.
What are the benefits offered by PhilHealth?
PhilHealth implements the National Health Insurance Program that aims to provide Filipinos with financial assistance and access to affordable health services. It covers hospital costs, subsidy for room and boarding, medicine, and professional services.
Can I use PhilHealth immediately?
To become eligible to PhilHealth benefits, members should have paid at least a total of nine (9) months premium contributions within the immediate twelve (12)- month period prior to the first day of confinement. The twelve (12)- month period is inclusive of the confinement month.
Can I use PhilHealth for check up?
The package covers preventive services like consultations, regular blood pressure measurements, counseling, periodic breast exams, and digital rectal exams. It can also be used for diagnostic examinations like complete blood count, chest x-ray, and urinalysis.
What if I stop paying my PhilHealth contribution?
What Happens if You Don't Pay PhilHealth Contributions? The good news is no one will be denied of PhilHealth coverage due to non-payment of premiums. If you miss a payment you will be billed monthly with interest as a consequence.
Can I use PhilHealth even if unemployed?
You can apply for PhilHealth voluntary membership even if you have no job as long as you can pay your monthly premiums. There's also no need to worry about PhilHealth requirements if you're unemployed. Just fill out the registration form and submit it with accurate information.
Can I still pay my PhilHealth contribution late?
Late payments for premium shall be computed with interests and/or surcharges. 2. The formula shall be: Interests and/or surcharges = Principal amount x 2% or Php200. 00, whichever is higher, compounded monthly based on the number of months delayed 3.
How many times can I use my PhilHealth?
PhilHealth members are entitled to a maximum of 45 days confinement per calendar year1. The qualified dependents of the member share another set of 45 days benefit per calendar year. However, the 45 days allowance shall be shared among them.
What is the disadvantage of PhilHealth?
Disadvantages: It's a bit harder for a freelance worker or self-employed starter as you would have to be the one going to PhilHealth or payment centers to pay and they have limited hospitals and doctors available (only government-owned hospitals usually accept PhilHealth).
What age is covered by PhilHealth?
Child or children - legitimate, legitimated, acknowledged and illegitimate (as appearing in birth certificate) adopted or stepchild or stepchildren below 21 years of age, unmarried and unemployed.
How many times can I use my PhilHealth benefits in a year?
You can avail of PhilHealth benefits anytime of the year as long as you fulfill the contribution requirements and benefit eligibility criteria disc...
How Can I use my PhilHealth for dependents?
To avail of PhilHealth benefits, you must have at least three months of contribution within the immediate six months before your dependent is confi...
Can senior citizens apply as PhilHealth members?
Yes, they can. Senior citizens can enroll by visiting the Office for the Senior Citizens Affairs or through a Local Health Insurance Office.
What PhilHealth Benefits are Available?
The agency typically pay parts of doctor’s professional fees, laboratory tests, and other medical costs.
Where does PhilHealth send benefits?
Once your benefits have been automatically deducted, PhilHealth will send a benefit payment notice to the address declared in your MDR. This details the actual payments made by PhilHealth relative to your claim or confinement.
What is PhilHealth and How Does It Work?
Established in 1995, PhilHealth aims to financially help Filipinos with their medical expenses. Contributions made by members and funding from both local and national governments enable PhilHealth to operate and aid its contributing members.
What is PhilHealth insurance?
The Philippine Health Insurance Corporation or PhilHealth is a government agency mandated to financially help Filipinos with their medical needs. As of 2015, about 88% of the country’s population are contributing members of the agency [1].
What is the first part of a PhilHealth claim?
Personal Information and Eligibility: The first part of the PhilHealth Claim Form requires the personal information of the PhilHealth member and/or the patient who will claim the benefit. This is important to identify the eligibility of the patient filing a claim.
How long do you have to contribute to PhilHealth?
To avail of PhilHealth benefits, you must have at least three months of contribution within the immediate six months before your dependent is confined. Claiming of benefits and its requirements are the same.
How old is a baby covered by PhilHealth?
PhilHealth members who are 24 to 36 weeks pregnant and at risk of premature birth are covered by PhilHealth. Additionally, premature newborns who are very small (500g to 2,499g fetal weight) at 24 weeks to less than 37 weeks (fetal age) are also covered by the agency.
How to pay PhilHealth contribution?
For employed PhilHealth Members, the PhilHealth Contribution would be automatically deducted from your salary. Half will come from your employer and half will come from you, the deducted amount will vary depending on the amount of salary you receive.
How to avail of PhilHealth Benefits?
There are conditions that have to be met in order for you to avail the benefits of PhilHealth when hospitalized, there are stated as follows:
What is philhealth for pregnant women?
PhilHealth Maternity Benefits are health benefits packages provided by the government to pregnant women, to cover their healthcare needs from prenatal to postpartum care . The benefits packages were formed with the help of health experts2to ensure safe pregnancy while factoring in the costs of giving birth. This benefit covers deliveries in hospitals and non-hospital birthing facilities, but not home deliveries.
What is the MCP package?
This is the benefits package available for mothers all throughout the pregnancy. MCP covers prenatal checkups, normal delivery, and postpartum care. For accredited hospitals, the coverage is PHP 6,500 and for accredited birthing homes, lying in or maternity clinics, the coverage is PHP 8,000.
What is the provision of essential newborn care?
Provisions of essential newborn care such as immediate drying of the baby, early skin-to-skin contact, cord clumping, non separation of mother and baby for early breastfeeding initiation, eye prophylaxis and vitamin K administration, weighing of the baby, and first doses of hepatitis and BCG vaccines.
How many copies of the PhilHealth membership form are needed?
Fill out two (2) copies of the PhilHealth Member Registration Form (PMRF) and attach 1×1 photo taken within the last six months;
What are dependents in PhilHealth?
The dependents can be any of the following: The legitimate spouse who is not enrolled under PhilHealth; Children, legitimate or illegitimate below twenty-one (21) years of age, who is unmarried, or without child/ren, and unemployed; A child who is twenty-one years of age or above suffering from a congenital disability;
Does PhilHealth print PBEF?
The hospital will then print the PhilHealth Benefit Eligibility Form (PBEF). If the PBEF says “YES”, it means the patient is entitled to the benefits. PhilHealth staff will then process the deduction from your hospital bills.
Where to submit PMRF?
Visit the OSCA of the city or municipality where you reside and submit the duly accomplished PMRF;
Who is a qualified dependent of a PhilHealth member?
Qualified dependent of a PhilHealth member who is also a senior citizen; Qualified dependent of a PhilHealth member who belongs to other membership categories.
Is it important to stay productive during retirement?
While it’s important to stay productive during your retirement years, there’s no way you can’t live a meaningful life without making your health a priority. Fortunately, the government assures senior citizens are well taken care of through the discounts and benefits offered by PhilHealth. DISCLAIMER: This article has been written ...
Is PhilHealth Free for Senior Citizens?
Yes. Thanks to Re public Act No. 10645 1, all senior citizens, indigent or not, are now automatically covered by PhilHealth.
How long do you have to pay for philhealth?
PhilHealth member must have paid at least 3 months of premiums/contributions within the immediate 6 months of confinement. For pregnancies, to avail of the newborn care package, dialysis, chemotherapy, radiotherapy and selected surgical procedures, PhilHealth member must have paid at least 9 months of contributions in the last 12 months.
What to do if you are not a member of PhilHealth?
If you’re not a member yet or you’re an inactive member of PhilHealth, I encourage you to continue your membership and pay your premiums continuously because you wouldn’t know when you’re going to need it. It would be a big help in case you or your dependents get sick or hospitalized.
How long do you have to stay in a hospital for a philhealth claim?
Attending physician (s) must also be PhilHealth accredited. Claim is within the 45 days allowance for room and board.
Do dependents need to be listed in the MDR?
If you are a dependent, make sure you are listed in the MDR.
Does PhilHealth take your hospital bill?
Once you have submitted the documents to the hospital before you get discharged, your PhilHealth benefits will be automatically deducted from your total hospital bill.
How to claim PhilHealth benefits?
Step 1 – Check on the coverage of the benefits offered by PhilHealth for its member or dependent who got admitted in a hospital. You may visit – PhilHealth Inpatient Benefit – Who Can Avail Financial Assistance. Step 2 – Visit the billing station and check on your hospital bill.
Why is PhilHealth deducted from hospital bill?
A huge part of the hospital bill may be deducted because of the membership and contribution remitted to the agency.
What is the Philippine Health Insurance Corp?
or more commonly called as PhilHealth is the state-run agency where a lot of people are relying when it comes to unforeseen medical emergencies. A huge part of the populace is a member of PhilHealth.