Key Takeaways
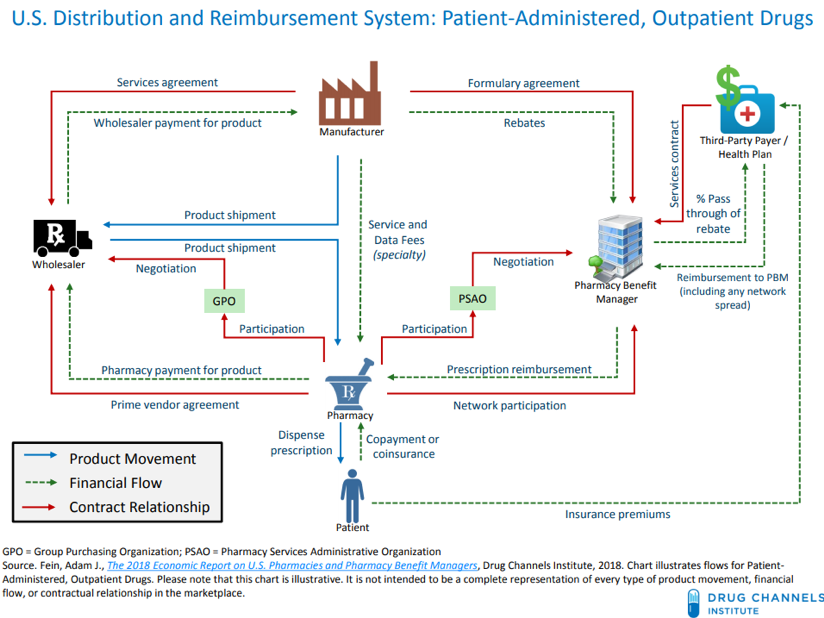
- Pharmacy benefit managers serve as the middlemen between drug companies and insurers.
- They negotiate discounts with drug makers and pass the cost savings on to insurers.
- These companies make money by up-charging the drugs or keeping some of the rebates.
- This sector of the industry is highly competitive and is characterized by consolidation.
What are the duties of a pharmacy manager?
What Are the Duties of a Pharmacy Manager?
- Supervisory Functions. A pharmacy manager typically oversees the work of subordinates, ensuring that employees perform tasks in accordance with corporate policies, industry practices and safety rules.
- Operating Duties. A pharmacy manager's operational functions are diverse. ...
- Regulatory Responsibilities. ...
- Technological Oversight. ...
- Education and Compensation. ...
How do pharmacy benefit managers affect you?
The top three PBMs by market share are:
- CVS Caremark, which manages 30% of the market;
- Express Scripts, which manages 23% of the market; and
- Optum Rx*, which manages 23% of the market.
Who is the largest pharmacy benefit manager?
In 2020, the top pharmacy benefit managers included CVS Health, Express Scripts, and OptumRx, to name a few. CVS Health had the largest share of the pharmacy benefit manager market in 2020. In total CVS Health held 32 percent of the market at that time. Pharmacy benefit managers are an important part of the prescription drug supply chain.
What is pharmacy benefit management (PBM)?
The term pharmacy benefit management (PBM) industry refers to a group of companies that serve as the middlemen between insurance companies, pharmacies, and drug manufacturers. PBMs are responsible for securing lower drug costs for insurers and insurance companies. They accomplish this by negotiating with pharmacies and drug manufacturers.

What is an example of a Pharmacy Benefit Manager?
Example of PBMs: CVS/caremark According to the CVS/caremark website: "Whether plan members access their prescriptions by mail or in one of our national network's more than 68,000 retail pharmacies, we provide the service and support needed to make sure the process goes smoothly.
How do pharmacy benefit managers make money?
PBMs mostly take spread pricing on generic drugs. PBMs also generate revenues from the direct and indirect remuneration fees (DIR) fees pharmacies pay, which include charges pharmacies pay to participate in a PBM's preferred network. There are also several new revenue streams emerging for PBMs.
What is the difference between an insurance company and a Pharmacy Benefit Manager?
The term pharmacy benefit management (PBM) industry refers to a group of companies that serve as the middlemen between insurance companies, pharmacies, and drug manufacturers. PBMs are responsible for securing lower drug costs for insurers and insurance companies.
What does a pharmacy benefits manager do quizlet?
pharmacy benefit managers (PBMs) are organizations that deliver, monitor & manage prescription drug benefits on behalf of a plan sponsor.
What is wrong with PBMs?
Because a portion of their profit is based on the rebate, PBMs rank drugs on their formularies based on the rebate amount rather than the lowest cost overall or drug efficacy. This encourages drug manufacturers to set artificially high list prices and offer steeper rebates rather than offer the lowest possible price.
How do I get PBM experience?
The primary qualifications for getting a job as a PBM pharmacist are having a pharmacist license and some experience working at a pharmacy. The requirements for getting the license vary by state but typically include a college degree in a relevant field, passing two exams, and providing some personal data.
Is GoodRx a PBM?
Essentially, GoodRx is a PBM-backed program that passes a portion of rebates and network discounts off list directly to patients at the point of sale. For a patient with insurance, benefit design and network rates can differ among PBMs.
How many pharmacy benefit managers are there?
Today, there are 66 PBM companies, with the three largest – Express Scripts (an independent publicly-traded company), CVS Caremark (the pharmacy service segment of CVS Health and a subsidiary of the CVS drugstore chain), and OptumRx (the pharmacy service segment of UnitedHealth Group Insurance) – controlling ...
Is Walgreens a PBM?
Walgreens Boots Alliance has officially launched its new specialty pharmacy and prescription mail services company with pharmacy benefit manager Prime Therapeutics , a PBM owned by 14 Blue Cross and Blue Shield plans.
Why is prescription management an important cost control quizlet?
Why is prescription management an important cost control? Prescription management is an important cost control because it increases the use of a formulary, a list of prescription drugs that health insurance will cover, to an inclusive approach to medications and medication administration.
What is a pharmacy benefit manager?
A pharmacy benefit manager is essentially a middleman service between the world's drugmakers and U.S. end payers, but healthcare investors need to understand far more about the unusual PBM industry. A pharmacy benefit manager (PBM) is a third-party administrator of prescription-drug programs for end payers, such as private insurers, ...
What is PBM in pharmacy?
Updated: Jul 21, 2017 at 12:05PM. A pharmacy benefit manager (PBM) is a third-party administrator of prescription-drug programs for end payers, such as private insurers, and Medicare Part D plans.
What are pharmacy benefit managers?
Pharmacy benefit managers, or PBMs, are companies that manage prescription drug benefits on behalf of health insurers, Medicare Part D drug plans, large employers, and other payers. By negotiating with drug manufacturers and pharmacies to control drug spending, PBMs have a significant behind-the-scenes impact in determining total drug costs for insurers, shaping patients’ access to medications, and determining how much pharmacies are paid. 1 PBMs have faced growing scrutiny about their role in rising prescription drug costs and spending.
What role do PBMs play in how much we spend on prescription drugs?
PBMs operate in the middle of the distribution chain for prescription drugs. That’s because they:
Why do PBMs get rebates?
Because they often receive rebates that are calculated as a percentage of the manufacturer’s list price, PBMs receive a larger rebate for expensive drugs than they do for ones that may provide better value at lower cost.
How do PBMs work?
PBMs operate in the middle of the distribution chain for prescription drugs. That’s because they: 1 develop and maintain lists, or formularies, of covered medications on behalf of health insurers, which influence which drugs individuals use and determine out-of-pocket costs 2 use their purchasing power to negotiate rebates and discounts from drug manufacturers 3 contract directly with individual pharmacies to reimburse for drugs dispensed to beneficiaries. 2
Why do PBMs need to reorient their business model?
Some experts think that PBMs also need to reorient their business model away from securing rebates and more toward improving value in pharmaceutical spending. For example, health plans and PBMs could do more to support physicians in prescribing the most cost-effective medications on their patient’s formularies.
Should PBMs keep rebates?
There is a lot of debate over whether PBMs should be able to keep the rebates they receive from drug manufacturers , which generally aren’t publicly disclosed. Some believe PBMs should be compelled to “pass through” all or a larger portion of these savings to health insurers and other payers.
Do PBMs have to pass rebates?
Alternatively, PBMs could be required to pass through rebates to patients. The federal government has, in fact, proposed requiring PBMs contracted with Medicare Part D plans to pass through to patients at least one-third of the rebates and price concessions they receive.
Why is it important to have a pharmacy benefit plan?
Having an effective pharmacy benefit strategy, and selecting the right PBM to meet an employer’s needs, is critical to ensuring the success of a benefits plan, optimizing spend, and protecting the well-being of employees.
What is a PBM in pharmacy?
What is a Pharmacy Benefit Manager (PBM) and how Does a PBM Impact the Pharmacy Benefits Ecosystem? Pharmacy Benefits Managers, also referred to as PBMs, are, in essence, the intermediaries of almost every aspect of the pharmacy benefits marketplace. Many people assume that pharmacy benefits come directly from the health insurance provider when, ...
What exactly do PBMs do?
PBMs have two main objectives: to curate pharmacy prescription benefits plan options; and to help patients achieve better health outcomes through greater access to appropriate medications.
How do PBMs work with Pharmaceutical Manufacturers?
The relationship between PBMs and pharmaceutical manufacturers is complicated. There are a number of financially-driven challenges that make interactions between drug companies and PBMs difficult to navigate and understand.
What does a PBM do?
PBMs negotiate with pharmaceutical companies to determine the level of rebates the company will offer for certain drugs — rebates are paid to the PBM. Depending on the contract between the PBM and employer, or plan sponsor, the PBM will pass all, some, or none of the rebate to the employer or plan sponsor.
Why are PBMs important?
It’s not always about money — PBMs play an important safety role within prescription benefits plans, too. Drug Utilization Review is a life-saving program that calls for the review of a drug to determine effectiveness, potential dangers, potential drug interactions, and mitigate other safety concerns. Since PBMs oversee their own pharmacy networks, they have access to a patient’s prescription history and can alert patients or physicians to potential negative drug interactions that could occur by mixing different prescriptions.
How long does a PBM contract last?
When an employer signs a contract with a PBM to design and maintain a prescription benefits plan, they typically contract for a three-year relationship. During the initial discovery phase, both parties work together, and in some cases with brokers and industry experts, to build their ideal pharmacy benefit plan by choosing from different deductibles, co-payments, co-insurances, and clinical programs.
