Most employers have a provision called " nonduplication of benefits," which means that the second plan will not duplicate benefits you've received under the first plan. Pick your plan Most employers are moving toward a provision called " nonduplication of benefits." That means the secondary plan won't duplicate benefits paid by the primary plan.
What does non duplication of benefits mean in dental insurance?
What does non duplication coordination of benefits mean in dental insurance? - Answers Non-Duplication of Benefits: Also known as a "carve out plan" is a plan designed to provide a certain level of cost sharing by the member.
What is the doctrine of non-duplication of benefits?
The doctrine of non-duplication of benefits intends to prevent this. For example, suppose a person has a home insurance policy that will provide $1,000 coverage for damage to their custom violin, as well as a separate, stand-alone personal property insurance policy that will also cover it for $1,000.
What is an example of duplication of benefits?
An example of a duplication of benefits is a renter who receives rental or housing assistance from the American Red Cross or the state of New York and also applies for FEMA rental or housing assistance for the same time period. FEMA cannot provide a benefit that is already being provided to the survivor.
What is a “duplication of benefits” from FEMA?
When determining the amount of federal disaster assistance an applicant may be eligible for, FEMA will verify there are no “duplication of benefits,” sometimes called double-dipping.
What does non-duplication mean in insurance?
Non-Duplication COB reduces/relieves the carrier from reimbursing any benefits. for services paid by another plan. If primary paid the same or more than what secondary carrier would have paid ( had they been primary), then second carrier is not responsible for any payment at all.
What does non duplicating mean?
Lack of duplication; failure to duplicate. noun.
What does non coordination of benefits mean?
Nonduplication COB - In the case of nonduplication COB, if the primary carrier paid the same or more than what the secondary carrier would have paid if it had been primary, then the secondary carrier is not responsible for any payment at all.
What is non dual coordination of benefits?
With non-duplication of benefits, the primary carrier pays its portion first and the secondary carrier, instead of paying the remainder, calculates what it would have paid if it were the primary carrier and subtracts what the other plan paid.
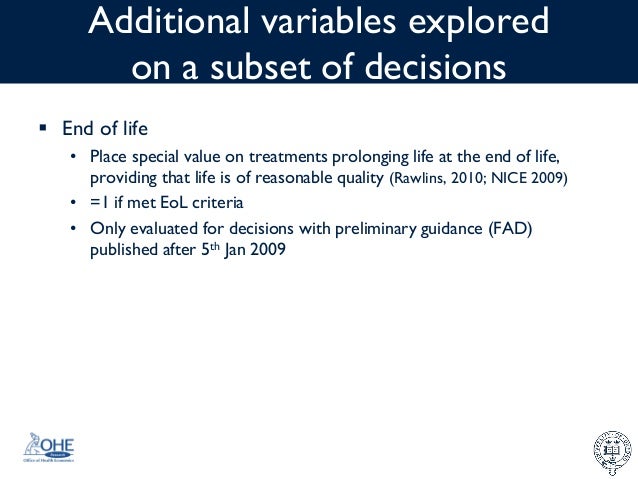
What are the 3 types of coordination of benefits for other insurance?
Understanding How Insurance Pays: Types of Coordination of Benefits or COBTraditional. ... Non-duplication COB. ... Maintenance of Benefits. ... Carve out. ... Dependents. ... When Does Secondary Pay? ... Allowable charge. ... Covered amount.
Is it worth it to have two dental insurances?
Having dual coverage doesn't double your benefits, but you might pay less for dental procedures than if you were covered under just one plan because treatment costs may be shared between your two carriers up to 100%.
What happens when you have 2 health insurance plans?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
How do you determine which insurance is primary and which is secondary?
The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer. The secondary payer only pays if there are costs the primary insurer didn't cover.
What does coordination of benefits mean?
Coordination of benefits (COB) allows plans that provide health and/or prescription coverage for a person with Medicare to determine their respective payment responsibilities (i.e., determine which insurance plan has the primary payment responsibility and the extent to which the other plans will contribute when an ...
Who is responsible for coordination of benefits?
Who is responsible for coordination of benefits? The health insurance plans handle the COB. The health plans use a framework to figure out which plan pays first — and that they don't pay more than 100% of the medical bill combined. The plan type guides a COB.
How does double vision coverage work?
When an employee has two different insurance plans at the same time, they have dual coverage. One plan will be designated as the primary plan and will pay first, the other will be designated as the secondary plan and will pay second.