What does full coverage from Medicaid means?
This program is able to provide full payment of both the Part A and Part B premiums and the annual deductible costs of these plans as well as co-insurance costs and deductible amounts also covered in full. This means that you should not be billed for any approved care you receive under Medicare Part A or Part B that is received at a Medicare-approved facility by an approved provider.
What items are not covered by Medicaid?
Some of the items and services that Medicaid does not cover include: Services that have been deemed by the peer review organization, DHS, Dental, or Optometric specialist not to be clinically essential. Services that are provided by direct relatives or members of the beneficiary’s home. Home remedies, nutritional supplements, vitamins ...
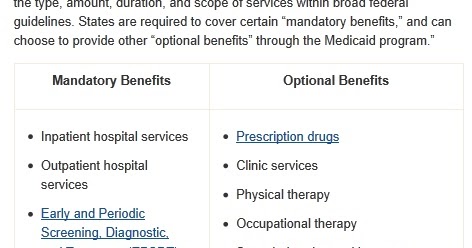
What are the most important Medicaid benefits?
These optional services may include but are not limited to: 2
- Case management
- Dental care (including dentures)
- Durable medical equipment
- Hospice care
- Mental health services
- Prescription medications
- Prosthetic devices
- Rehabilitation services (including physical therapy and occupational therapy)
- Telemedicine
- Vision care (including eyeglasses)
Which health plan is best for Medicaid?
"That's the essential value of care coordination at its best. We are delighted to partner ... benefit from their expertise." ACAP-member plans serve more than 20 million enrollees through Medicaid, Medicare, Health Insurance Marketplaces, the Children's ...

What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What is the most you can make with Medicaid?
The state also has Medicaid programs for assisted care and children with complex medical needs. Income requirements: For Medicaid coverage a single adult is capped $1,482 per month and families of four can make $3,048 per month. Single aged or disabled adults over 65 have an income cap of $847 and $1,211 for couples.
What is the lowest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What does NYS Medicaid cover?
New York Medicaid Benefits. New York Medicaid benefits include regular exams, immunizations, doctor and clinic visits, relevant medical supplies and equipment, lab tests and x-rays, vision, dental, nursing home services, hospital stays, emergencies, and prescriptions.
What is the income limit for food stamps 2021?
$1,500 earned income + $550 social security = $2,050 gross income. If gross monthly income is less than the limit for household size, determine net income. $2,050 is less than the $2,871 allowed for a 4-person household, so determine net income.
What is the Medi-Cal income limit for 2021?
A single adult can earn up to $17,775 in 2021 and still qualify for Medi-Cal. A single adult with one dependent can earn up to $46,338 annually and the child will still be eligible for Medi-Cal.
What is considered low income for a single person in 2021?
2021 POVERTY GUIDELINES FOR THE 48 CONTIGUOUS STATES AND THE DISTRICT OF COLUMBIAPersons in family/householdPoverty guideline1$12,8802$17,4203$21,9604$26,5005 more rows
How can I hide money from Medicaid?
5 Ways To Protect Your Money from MedicaidAsset protection trust. Asset protection trusts are set up to protect your wealth. ... Income trusts. When you apply for Medicaid, there is a strict limit on your income. ... Promissory notes and private annuities. ... Caregiver Agreement. ... Spousal transfers.
Who is qualified for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
What is the monthly income limit for Medicaid in NY?
Eligibility and CostFamily ContributionsMonthly Income by Family Size*17Free Insurance$1,811$5,587$9 Per Child Per Month (Maximum of $27 per family)$2,515$7,754$15 Per Child Per Month (Maximum of $45 per family)$2,832$8,7324 more rows
Does Medicaid cover surgery?
Medicaid does cover surgery as long as the procedure is ordered by a Medicaid-approved physician and is deemed medically necessary. Additionally, the facility providing the surgery must be approved by Medicaid barring emergency surgery to preserve life.
Does Medicaid cover prescriptions in NY?
The New York State Medicaid Pharmacy program covers medically necessary FDA approved prescription and non-prescription drugs for Medicaid fee-for-service and Medicaid Managed Care enrollees.
Basic Eligibility Requirements to Get Coverage
The basic requirements to qualify for any Medicaid benefits in Mississippi are: 1. You must be a citizen of the United States or a qualified alien....
Mississippi Medicaid and The Affordable Care Act
The Affordable Care Act (ACA) creates insurance affordability programs as a way to get health coverage at no cost or lower cost than purchasing cov...
Notice of Privacy Practices
The Health Insurance Portability and Accountability Act (HIPAA) notice of privacy practices describes how medical information about you may be used...
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
What is not covered by Medicare?
Offers benefits not normally covered by Medicare, like nursing home care and personal care services
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover health care?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is the Medicaid age limit?
The Affordable Care Act of 2010 created the opportunity for states to expand Medicaid to cover nearly all low-income Americans under age 65 . Eligibility for children was extended to at least 133% of the federal poverty level (FPL) in every state (most states cover children to higher income levels), and states were given the option to extend eligibility to adults with income at or below 133% of the FPL. Most states have chosen to expand coverage to adults, and those that have not yet expanded may choose to do so at any time. See if your state has expanded Medicaid coverage to low-income adults.
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
What are the factors that determine if you qualify for medicaid?
The benefits you qualify for depends on your income, age, family size and situation. These factors also determine if you qualify for full Medicaid benefits, reduced coverage or limited benefits. Additionally, some extra services beyond basic Medicaid are available through waiver programs.
What is the Affordable Care Act in Mississippi?
The Affordable Care Act (ACA) creates insurance affordability programs as a way to get health coverage at no cost or lower cost than purchasing coverage on your own. In Mississippi, these programs include Mississippi Medicaid health benefits (Medicaid and CHIP) and health coverage through a federally facilitated marketplace (FFM).
Do I need to be a resident of Mississippi to get medicaid?
You must be a resident of Mississippi. You must meet requirements for age and/or disability, income and other Mississippi Medicaid eligibility requirements such as resources for certain aged, blind or disabled coverage groups. You must file an application form. You must provide requested verification within the allowed time limits.
Can you get cost sharing reductions through FFM?
Certain households will also qualify for cost-sharing reductions for out-of-pocket expenses for insurance through the FFM. In order to qualify for insurance through the marketplace, an individual must not be eligible for Medicaid, CHIP or affordable job-based health coverage, as determined by the FFM. Individuals who apply for health coverage ...
Can I apply for medicaid through FFM?
No separate application is needed to apply for Mississippi health benefits.
What if I have full coverage for medicaid?
What if I have full coverage from my state Medicaid program? If you have full coverage from your state Medicaid program and you are eligible for Medicare , Medicare will automatically enroll you in Medicare prescription drug coverage if you have not already chosen to do so.
Does Medicare cover prescription drugs?
Medicaid will still cover other care that Medicare doesn't cover. In some limited cases, Medicaid will add to Medicare drug coverage. You can switch to another Medicare drug plan each month.
What is considered minimum essential coverage?
Find out if your Medicaid program counts as minimum essential coverage. Most Medicaid programs are considered "minimum essential coverage" (also known as qualifying health coverage ). This means they meet the requirement for having health coverage under the health care law.
What to do if someone in your household is covered by the programs above?
What to do: If anyone in your household is covered by the programs above, IMMEDIATELY end their Marketplace coverage with premium tax credits. See how to end a Marketplace insurance plan.
Can you deduct medical expenses on medicaid?
Medicaid for medically needy individuals if you qualify for comprehensive coverage without needing to deduct medical expenses from your income to meet the state’s medically needy income level (spend down). (Medically needy programs are for people with high medical expenses who wouldn’t otherwise qualify for Medicaid because their income is too high.)
Does Medicaid count as essential coverage in the District of Columbia?
See how to end a Marketplace insurance plan. They can enroll in a Marketplace plan, but only at full price. Medicaid that DOESN’T count as “minimum essential coverage” in District of Columbia. If anyone in your household is covered by only the following programs, they do not have minimum essential coverage.
Do you have to have minimum essential coverage?
If anyone in your household is covered by the following programs, they do have minimum essential coverage. This means they are not eligible for premium tax credits and other savings with a Marketplace plan.
Does medicaid count as essential coverage?
If your Medicaid program DOESN’T count as minimum essential coverage: You are eligible for premium tax credits and other savings on a Marketplace insurance plan, if you qualify based on your income and other criteria.
Can you get a premium tax credit for Medicaid?
If your Medicaid program counts as minimum essential coverage: You are not eligible for a premium tax credit or other savings to enroll in a Marketplace insurance plan. You should immediately end Marketplace insurance for anyone in your household who is enrolled in these Medicaid programs and is also using premium tax credits with a Marketplace plan.
What is limited benefit package?
Limited Benefit Package for Adults. Adults (age 21 and over) receiving federally matched Medicaid who are not in a nursing facility or receiving based on blindness or pregnancy have a “limited benefit package”. The coverage limitations are:
What is the provider resource guide?
The Provider Resource Guide contains MO HealthNet division contact information including provider communication, pharmacy/clinical services, exception process, participant services, and a list of ME Codes with benefit package information.
How to find out if transplant is covered by MO HealthNet?
transplants. Call the MO HealthNet Participant Services Unit,1-800-392-2161, to find out if a specific procedure is covered. Individuals Eligible for Full Comprehensive Medicaid Benefit package: Children and young adults under age 21 receive the full comprehensive benefit package, unless they are:
What does ME 80 89 cover?
Uninsured Women’s Health Services (ME 80,89) only covers family planning and testing for STDs.
Who authorizes home and community based waiver services?
home and community based waiver services (authorized by DMH Division of Developmental Disabilities or Department of Health and Senior Services).
Can you opt out of managed care if you have a disability?
Participants in these categories have the option of opting out of managed care if they have a disability.
Is behavioral health covered by state custody?
For children state custody or adoption subsidy, all behavioral health services are covered fee-for-service.
What does 0% mean on Medicaid?
If “0%” appears, that means individuals may not qualify for Medicaid in that state based on income alone and must meet other criteria, such as being pregnant or disabled.
What is FPL in Medicaid?
FPL is used to determine eligibility for Medicaid, certain welfare benefits and other assistance programs. The FPL is computed by the U.S. Census Bureau and can be adjusted every year based on inflation.
How many states do not grant Medicaid?
There are 13 states that do not grant Medicaid access to individuals based on income alone.
How long does it take to get approved for medicaid?
Contact your state Medicaid program in order to apply for Medicaid. Applications are generally reviewed and approved within 90 days and typically are reviewed sooner.
Can you have both Medicare and Medicaid?
If you qualify for both Medicare and Medicaid, you are considered “dual eligible.” In this case, you may qualify for a certain type of Medicare Advantage plan called a Dual Eligible Special Needs Plan (D-SNP). D-SNPs are designed to meet the specific needs of people who have Medicaid and Medicare.
Does each state have its own medicaid program?
Each state runs its own Medicaid programs with its own set of qualifying criteria.
Is Medicaid a federal program?
While Medicaid is a federal program, eligibility requirements can be different in each state.
