Can glp-1ras improve cardiac function?
Accordingly, it is suggested that GLP-1RAs have properties of alleviating MI and repairing damaged cardiac tissue to improve cardiac function (Figure (Figure11). Effects of GLP-1RAs on heart failure Myocardial remodeling has a critical role in heart failure following MI. Disturbances in cardiac calcium metabolism are a hallmark of heart failure.
Do GLP-1 agonists have metabolic and cardiovascular benefits?
Metabolic and cardiovascular benefits of GLP-1 agonists, besides the hypoglycemic effect (Review) Patients with type 2 diabetes exhibit higher cardiovascular risk than normal individuals. Optimal blood glucose levels are rarely achieved in diabetic patients.
Can glp-1ra (hypoglycemic peptide 2) prevent cardiomyopathy?
Furthermore, a new orally bioavailable GLP-1RA, oral hypoglycemic peptide 2 (OHP2), can confer protective effects on diabetic cardiomyopathy through rescuing cardiac lipotoxicity by inhibiting Rho (the small GTPase) kinase (ROCK)/PPARα pathway 89, 90(Figure (Figure11). Molecular mechanisms of GLP-1RA-mediated cardiovascular actions
What is the role of GLP-1R in angioplasty?
GLP-1R can also suppress cardiac hypertrophy induced by Ang II through attenuating the Nox4-histone deacetylase 4 (HDAC4) axis 162. Apart from these actions, GLP-1RAs ameliorate cardiac fibrosis induced by abdominal aortic constriction via interfering with Ang II type 1 receptor signaling 163.

Which GLP-1 receptor agonist has the strongest evidence for use in patients with cardiovascular disease?
The strongest evidence lies with semaglutide, liraglutide, dulaglutide and albiglutide, followed by exenatide once-weekly (although these results did not reach significance), with lixisenatide being neutral in terms of cardiovascular outcomes.
Do GLP-1 agonists have cardiovascular benefit?
GLP-1 agonists may have beneficial effects on cardiovascular outcomes, by modulating other risk factors, such as endothelial dysfunction, arterial blood pressure, dyslipidemia, and platelet function (30).
Does dulaglutide have cardiovascular benefit?
Trulicity® (dulaglutide) is the first and only type 2 diabetes medicine approved to reduce cardiovascular events in adults with and without established cardiovascular disease.
Which diabetic medication has cardiovascular benefit?
New medications like empagliflozin and liraglutide improve not only CV mortality but also all-cause mortality in diabetic patients with CVD. The FDA has approved specific labels for both empagliflozin and liraglutide to reduce the risk of CV death in adults with diabetes and CVD.
Does Ozempic have cardiovascular benefits?
The combined data from these trial show that Ozempic, compared to placebo (a nothing pill), reduced the risk of heart attack, stroke, and heart-related death by a whopping 24%.
Does lixisenatide have cardiovascular benefit?
In patients with type 2 diabetes and a recent acute coronary syndrome, treatment with the GLP-1–receptor agonist lixisenatide, added to conventional therapy, was not associated with a significant difference in rates of cardiovascular events as compared with conventional therapy plus placebo.
Does Trulicity affect your heart?
Type 2 Diabetes Drug Trulicity Cuts Risk for Heart Events by 12 Percent. In a clinical trial, the medication, whose generic name is dulaglutide, also reduced the risk for kidney problems by 15 percent.
Do GLP-1 receptor agonists care if you have heart failure?
GLP-1 RAs have no effect on the risk of HF hospitalization, which suggests that they are safe to use, but not beneficial in preventing HF in patients at risk.
Does exenatide have CV benefits?
Among patients with type 2 diabetes and confirmed CVD at baseline, treatment with once-weekly exenatide reduced the risk for major adverse CV events, with no new or overall safety concerns related to cardiac events, according to a prespecified subgroup analysis of the EXSCEL study.
Does victoza help with heart disease?
Victoza® helps lower the risk of major cardiovascular events. Talk to your health care provider about how Victoza® not only lowers A1C, but also reduces the risk of major CV events such as heart attack, stroke, or death in adults with type 2 diabetes with known heart disease.
What is the best medicine for the heart?
Modern heart drug therapy includes the following “big six” medications:Statins — to lower LDL cholesterol. ... Aspirin — to prevent blood clots. ... Clopidogrel — to prevent blood clots. ... Warfarin — to prevent blood clots. ... Beta-blockers — to treat heart attack and heart failure and sometimes used to lower blood pressure.More items...•
How does empagliflozin help the heart?
"Results from the EMPEROR-Reduced trial show that, when given to adults with heart failure with reduced ejection fraction, empagliflozin reduces the number of heart failure hospitalizations while slowing the decline of kidney function. These results are highly statistically significant and clinically important."
What are the effects of GLP-1?
In summary, GLP-1 has important postprandial physiological effects that include stimulation of insulin secretion in a glucose-dependent manner, suppression of glucagon secretion, decreased rate of gastric emptying, and suppression of appetite. Multiple GLP-1 receptor agonists have been developed for treatment of type 2 diabetes. All of the five currently clinically available drugs produce significant improvement in glycemic control in association with modest weight loss, but so far only liraglutide 1.2 to 1.8 mg SQ daily has been demonstrated to reduce the risk of cardiovascular events. The Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) of the FDA recently voted in favor of adding information from the LEADER trial to the labeling for liraglutide. Liraglutide is also FDA approved at the higher dose of 3 mg SQ daily for the purpose of weight loss. Long-acting exenatide and lixisenatide were non-inferior to placebo in relation to cardiovascular events, but neither demonstrated a significant reduction in cardiovascular events. Cardiovascular outcomes data are not yet available for albiglutide and dulaglutide, but the experimental GLP-1 agonist semaglutide has been shown to reduce the risk of cardiovascular events compared to placebo. It is possible that the differences in results from the various cardiovascular outcomes trials are related to differences in study populations or study design, but these features do not provide a clear explanation for the absence of a significant reduction in cardiovascular events with lixisenatide and extended release exenatide. Further studies are needed to clarify whether cardiovascular event reduction in response to treatment with GLP-1 receptor agonists is a class effect and to elucidate the mechanisms by which liraglutide and semaglutide reduce cardiovascular events. In the meantime, this class of drugs provides an effective option for treatment of hyperglycemia and mediating modest weight loss in type 2 diabetes.
How much liraglutide should I take daily?
The median dose of liraglutide was 1.78 mg daily, which reflected the target dose of 1.8 mg daily or the highest tolerable dose. The HgbA1c concentration decreased by 0.4 (95% CI –0.45 to –0.34) at 36 months, body weight modestly decreased by 2.3 kg (95% CI –2.5 to –2.0), and systolic blood pressure decreased by –1.2 mm Hg (95% CI –1.9 to –0.5) during treatment with liraglutide compared to placebo, all P < 0.05.
What is the hazard ratio of liraglutide?
The hazard ratio for the primary cardiovascular outcome was significantly reduced in the liraglutide group compared to placebo, with hazard ratio 0.87 (95% CI 0.78 to 0.97, P = 0.01). The expanded composite cardiovascular outcome (consisting of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke, coronary revascularization, or hospitalization for unstable angina pectoris or heart failure) was also significantly reduced, with a hazard ratio of 0.88 (95% CI 0.81 to 0.96, P = 0.005). The rate of cardiovascular mortality was significantly lower in the liraglutide group, with hazard ratio 0.78 (95% CI 0.66 to 0.93, P=0.007), and total mortality (death from any cause) was also significantly lower in the liraglutide group, with hazard ratio 0.85 (95% CI 0.74 to 0.97, P = 0.02). The individual rates of nonfatal myocardial infarction, nonfatal stroke, and hospitalization for heart failure were nonsignificantly lower in the liraglutide group. The rate of incident nephropathy was significantly reduced by liraglutide compared to placebo (HR 0.78, 95% CI 0.67 to 0.92, P = 0.003), but the incidence of retinopathy was unaffected (HR 1.15, 95% CI 0.87 to 1.53, P = 0.33).
What are the results of the Leader trial?
To summarize the results of the LEADER trial, the data demonstrated significant improvements in glycemic control, decreased incidence of severe hypoglycemia, modest weight loss, modest lowering of systolic blood pressure, decreased incidence of nephropathy, and a reduction in composite cardiovascular endpoints as well as total and cardiovascular mortality in high risk patients with type 2 diabetes treated with liraglutide compared to placebo. The rates of any adverse event (62.3 vs. 60.8%) or severe adverse event (32.2 vs. 32.8%) were not significantly different between the liraglutide and placebo treatment groups.
Does lixisenatide help with cardiovascular disease?
The results of another cardiovascular outcomes trial using lixisenatide also did not show cardiovascular benefit. In the Evaluation of Cardiovascular Outcomes in Patients With Type 2 Diabetes Mellitus After Acute Coronary Syndrome During Treatment With Lixisenatide (ELIXA) trial, 6068 patients with type 2 diabetes and cardiovascular disease were treated with lixisenatide for a median duration of 2.1 years. 11 The subjects in this trial had a mean age of 60.3 +/- 9.6 years and HgbA1c 7.6 +/- 1.3%. The study demonstrated that lixisenatide was non-inferior to placebo for cardiovascular outcomes, but the primary composite cardiovascular outcome was not significantly reduced in the lixisenatide group (HR 1.02 ; 95% CI 0.89 to 1.17).
Is liraglutide FDA approved?
The Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) of the FDA recently voted in favor of adding information from the LEADER trial to the labeling for liraglutide. Liraglutide is also FDA approved at the higher dose of 3 mg SQ daily for the purpose of weight loss.
Is semaglutide safe for diabetics?
In contrast, the experimental GLP-1 receptor agonist, semaglutide, has been demonstrated to have cardiovascular benefit. The randomized placebo-controlled Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes (SUSTAIN-6) was designed to demonstrate the noninferiority of semaglutide compared to placebo for cardiovascular safety in 3297 patients with type 2 diabetes. 12 The study population consisted of 3297 subjects with type 2 diabetes and a mean age of 64.6 +/- 7.4, baseline HgbA1c 8.7 +/- 1.5, and baseline cardiovascular disease in 83% of the subjects. The results demonstrated a significant reduction in cardiovascular events in patients treated with semaglutide 0.5 or 1.0 mg subcutaneously weekly (hazard ratio 0.74; 95% confidence interval [CI] 0.58 to 0.95). Rates of nephropathy were lower, but complications of retinopathy were higher with semaglutide compared to placebo. Semaglutide is not yet FDA approved for clinical use in the United States.
What is GLP-1RA?
GLP-1 is a gut-derived insulin agonist with the ability to suppress glucagon release and stimulate insulin secretion through targeting α-cells and β-cells, respectively 5. Likewise, GLP-1RAs can lower postprandial glycemia predominantly by slowing gastric emptying and promoting weight loss 6, 7. GLP-1RAs may improve endothelial cell function via anti-inflammatory and vasodilatory properties. Also, anti-proliferative effects on smooth muscle cells and anti-inflammatory effects on macrophages may contribute to the protection against the development and progression of atherosclerosis 8-10. In consideration of the dual roles of GLP-1RAs in hypoglycemic effects and preventing CVD among T2DM patients, we reviewed the cardiovascular effects and molecular mechanisms of GLP-1RAs in CVOTs, animal models and cultured cells, and discuss how these findings transform pharmacotherapies for T2DM, and even expand the indication of this important category of anti-diabetic drugs to CVD patients without diabetes.
Does GLP-1RA have a side effect?
Based on the above pharmacological characteristics of categories of GLP-1RAs agents, despite slight adverse gastrointestinal side effects, it is clear that GLP-1RAs agents have efficacy in cardiovascular protection without untoward hypoglycemia.
Does GLP-1RA reduce MI?
Multi-country, multi-center long-term cardiovascular outcome trials (CVOTs) confirmed that GLP-1RAs decrease cardiovascular mortality and provide cardiovascular benefits to reduce the incidence of MI or non-fatal stroke 3. For example, in the LEADER trial, when compared with placebo, liraglutide decreased the incidence of major cardiovascular events (MACE) by 13%, cardiovascular death by 22% and all-cause death by 15% among T2DM patients with CVD, on a standard treatment basis 4. In addition, liraglutide provided multiple additional benefits by reducing the incidence of hypoglycemia, lowering HbA1c and functioning through multiple mechanisms to better control multiple causes of MACE, such as blood lipids, BP as well as body weight (BW).
Is dodecaplatin FDA approved?
By February 21, 2020, dodecaplat in®(dulaglutide) is the first and only FDA-approved anti-diabetic drug for primary and secondary prevention to alleviate the risk of MACE 25.
Does taspoglutide reduce LDL?
In 2015, a randomized controlled trial showed that taspoglutide can reduce total cholesterol, LDL-C and triglycerides 34. Among new-onset patients with diabetes receiving standard statin therapy, liraglutide together with metformin improved lipid distribution of LDL and C-reactive protein (CRP) in atherosclerosis 35. Studies have also reported that under the conditions of comparable glycemic control, liraglutide (1.2 mg/d) alone was more effective than liraglutide with metformin or metformin alone on lipid metabolism and cardiovascular protection 36.
Does GLP-1RA lower blood glucose?
All five long-acting GLP-1RAs can reduce glucose levels and BW 4, 22, 23, 26, 27. In SUSTAIN 3, SUSTAIN 7 and SUSTAIN 10, the GLP-1RAs semaglutide reduced HbA1c by up to 1.8%, achieved the glycemic control target of HbA1c in 80% of the intervention group, and reduced BW by up to 6.5 kg, outcomes which were superior to liraglutide, exenatide and dulaglutide 28-30. In the LEAD-5 trial, liraglutide (1.8 mg once daily) reduced HbA1c more than insulin glargine during the treatment period (26 weeks) 31. The results of AWARD-CHN2 showed that the reduction of FPG by dulaglutide was similar to insulin glargine. In addition, post-prandial blood glucose reduction by dulaglutide was superior to insulin glargine. In addition to this, dulaglutide can greatly stabilize and decrease blood glucose levels 32.
Can you check blood sugar in pharmacies?
Patients walk into pharmacies all the time to check their blood pressure, check their blood glucose, to see if something may be wrong with their blood glucose monitor. It’s a great opportunity to check their blood sugar.
Can you bring a glucose monitor into a pharmacy?
We often have patients that bring their blood glucose monitor into pharmacies to download their reading prior to their provider’ s office visit, which we actually recommend for all our diabetes patients. Bring in your monitor and we’ll download the readings, that way you can take it into your prescriber.
Does rosiglitazone increase myocardial infarction?
As more diabetes drugs came to the market, there was concern regarding the effect of these drugs on cardiovascular risk, particularly with the drug rosiglitazone, which was associated with a significant increase in the risk of myocardial infarction. 14 Given these concerns, in 2008 the FDA came out with a recommendation that new glucose-lowering medications for diabetes are shown to not increase cardiovascular risk. 15 This recommendation led to long-term prospective cardiovascular outcomes trials (CVOTs) for new diabetes drugs. In this process, several medications within the GLP-1 RA class have not only shown non-inferiority but have also shown superiority in terms of their cardiovascular outcomes, which we will present here. As studies begin to show important cardiovascular benefits among certain drug classes, the American Diabetes Association (ADA) has now incorporated this consideration into its 2019 guidelines on diabetes treatment. 16
Is HgA1C high risk?
This trial had a high percentage of patients with underlying cardiovascular disease and it also had one of the highest baseline HgA1c values ( table 2 ), suggesting a very high-risk population. This was the first study to show cardiovascular benefit, although this benefit may not apply for lower risk patients or those without established cardiovascular disease.
Does glycaemic control reduce microvascular complications?
Although it has been shown that improved glycaemic control can reduce the microvascular complications of diabetes, 7 its effect on macrovascular complications is less clear, 8 and cardiovascular disease remains the number one cause of death in patients with T2D. 9 The main long-term data we have looking at glycaemic control in patients with T2D on macrovascular outcomes are from the UKPDS (UK Prospective Diabetes Study) and VADT (Veterans Affairs Diabetes Trial)—although neither study showed clear cardiovascular mortality benefit initially, the 10-year follow-up to UKPDS did suggest a potential ‘legacy effect’ of early tight glycaemic control leading to later reductions in myocardial infarction and death, 10 but no similar reduction in cardiovascular mortality was seen in the follow-up VADT. 11 Further complicating this is the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial, published in 2008, which found that more intensive glycaemic control resulted in no reduction in cardiovascular events and in fact increased overall mortality. 12 A 9-year follow-up to this study showed the intensive group had no difference in overall mortality but did have increased cardiovascular-related deaths. 13
Is GLP-1 a RA?
Certain glucagon-like peptide 1 receptor agonists (GLP-1 RAs) have shown benefit compared with placebo in decreasing the risk of composite cardiovascular outcomes in patients with type 2 diabetes (T2D). Current guidelines have changed to recommend GLP-1 RA as the preferred therapy after metformin in patients with T2D with established cardiovascular ...
Does semaglutide improve HgA1C?
This trial also had one of the highest baseline HgA1c ( table 2) compared with other trials. The trial had the largest improvement of HgA1c with semaglutide compared with control (−0.7% and −1.0%, semaglutide 0.5 mg and 1.0 mg compared with control), questioning whether the cardiovascular benefit was seen from the medication itself or the improved glycaemic control.
What is GLP-1 RA?
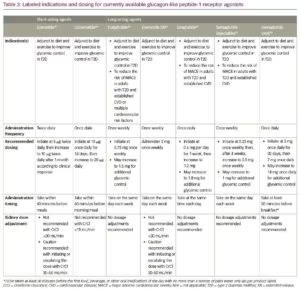
Glucagon- like peptide 1 receptor agonists (GLP-1 RAs) are emerging as an important therapy to consider for patients with type 2 diabetes (T2D) given this class of treatment’s ability to reduce glycated haemoglobin and their associated weight loss and low risk for hypoglycaemia. Additionally, seven cardiovascular outcomes trials (CVOTs) have been performed in the past 4 years using lixisenatide, liraglutide, semaglutide, exenatide, albiglutide, dulaglutide and oral semaglutide. All have found non- inferiority for cardiovascular outcomes, with many finding superiority of these drugs. These findings have transformed our guidelines on pharmacological treatment of T2D. This review article will discuss GLP-1 RA therapy, review the seven CVOTs reported to date and discuss the implications on current guidelines and therapies going forward.
How many GLP-1 CVOTs are there?
To date, there have been seven GLP-1 RA CVOTs as previously outlined. Of these, all have shown non- inferiority, and liraglu-tide, subcutaneous semaglutide, albigultide and dulaglutide have shown significant reductions in composite cardiovascular outcomes. Lixisenatide had the highest risk population, with 100% of participants having had an acute coronary event in the past 180 days, and had similar incidence of the primary composite outcome around 13%, similar to the other higher risk CVOTs, but interestingly did not find a significant difference in the primary outcome.17 There is some thought that the short half- life of lixisenatide compared with the other medications (table 1) may contribute to its lack of cardiovascular benefits. The EXSCEL study also found no significant difference in cardio-vascular outcomes with once- weekly exenatide20; however, it should be noted that the EXSCEL study had no run- in period to improve adherence to the medication regimen, and therefore the discontinuation rate was higher, which could have attenuated the significance. Overall, the EXSCEL study also had slightly shorter duration and lower HgA1c, although given the incidence of cardiovascular events was similar to other studies, this should not have affected the outcome.