
Create & Submit Application
- Apply online Visit www.gateway.ga.gov. Select Apply for Benefits to begin. Select Medical Assistance as a program. Follow the online prompts to apply for Medicaid.
- Apply by phone You can apply by phone by calling 877-423-4746. After your call, you may need to provide additional information or documentation.
- Apply in person You can apply in person through your county Division of Family and Children Services (DFCS) office. Be sure to bring all required documentation for your visit.
- Apply by mail You can apply by mail by calling 877-423-4746 and requesting to have forms mailed to you. ...
How much does Medicaid pay for a nursing home?
Medicaid will pay 100% of the cost of nursing home care for its beneficiaries. However, to be eligible for Medicaid nursing home care, the patient must have very limited income and very few financial assets (ballpark limits are assets valued under $2,000 and monthly income under $2,382). Medicaid eligibility criteria is state-specific.
Are nursing homes covered by Medicaid?
Types of Medicaid that Cover Nursing Homes. Nursing home Medicaid is also called Institutional Medicaid and is available for eligible Americans in every state. Nursing Home Medicaid is different from the other forms of Medicaid long term care, specifically Medicaid Waivers and Aged, Blind, and Disabled Medicaid (ABD is also called Regular Medicaid). HCSB waivers and ABD Medicaid can cover the some but not all of the costs of medical and personal care services in a home or assisted living ...
How does Medicaid cover nursing home?
Medicaid is a federal-state joint program which offers health insurance coverage to low-income seniors, children, and those who have disabilities. It also covers care inside a nursing home for the ...
How to get into a nursing home on Medicare?
- The patient requires medical care that’s not available in a nursing home (e.g. ...
- The patient’s condition has improved and they no longer require skilled nursing care
- The patient jeopardizes the health and safety of others in the nursing home
- The patient has not paid for care in at least 15 days
- The nursing home plans to cease operations
How to apply for medicaid for nursing home?
First, the applicant applies for Medicaid, which they can do online or at any state Medicaid office.
How many states have Medicaid eligibility for nursing home care?
Medicaid Eligibility for Nursing Home Care. To be eligible for nursing home care, all 50 states have financial eligibility criteria and level of care criteria. The financial eligibility criteria consist of income limits and countable assets limits. These limits change annually, change with marital status, and change depending on one’s state ...
Why do nursing homes prefer private pay?
The reason for this is because private pay residents pay approximately 25% more for nursing home care than Medicaid pays.
How much will Medicaid pay in 2021?
In 2021, the nationwide average private payer pays $255 per day for nursing home care while Medicaid pays approximately $206 per day. Being Medicaid eligible and finding a Medicaid nursing home is often not enough to move a loved one in. Read about how to get into a nursing home .
What is a short term nursing home?
Short-term nursing homes are commonly called convalescent homes and these are meant for rehabilitation not long term care. Be aware that different states may use different names for their Medicaid programs. In California, it is called Medi-Cal. Other examples include Tennessee (TennCare), Massachusetts (MassHealth), and Connecticut (HUSKY Health).
What is a trustee in Medicaid?
A trustee is named to manage the account and funds can only be used for very specific purposes, such as contributing towards the cost of nursing home care. Assets. In all states, persons can “spend down” their assets that are over Medicaid’s limit. However, one needs to exercise caution when doing so.
Can a married couple get Medicaid for nursing home?
Note for Married Couples – While a single nursing home Medicaid beneficiary must give Medicaid almost all their income for nursing home care, this is not always the case for married couples in which only one spouse needs Medicaid-funded nursing home care.
How to determine if you are eligible for medicaid?
There are 3 relatively simple approaches to determine if you or a loved one is eligible 1) Read national guidelines 2) Read state specific guidelines 3) Take a non-binding Medicaid eligibility pre-screen.
What are the eligibility groups for Medicaid?
For the vast majority of seniors in most states, there are 3 relevant eligibility groups. 1) Nursing Home Medicaid – also called “Institutional Medicaid”, provides for nursing home care only. 2) Home and Community Based Services / Waivers – sometimes ...
What to do if you determine a Medicaid candidate is not automatically eligible for Medicaid?
If you determine the Medicaid candidate is not automatically eligible for Medicaid, you should read about Medicaid planning, understand the different types of Medicaid planning assistance or complete this form to find a Medicaid planner.
How long does it take for a medicaid application to be approved?
Medicaid offices, by law, have a maximum of 90 days to review a Medicaid application, make an approved / denied determination and to notify the applicant. However, there is no way for applicants to enforce this law and sometimes state Medicaid offices do take longer than 90 days.
How does misstep affect Medicaid?
Any missteps in the application process can result in lengthy delays in receiving an approval or denial from your county Medicaid office. Following these steps will help to make the process less burdensome, less error prone and can reduce the time it takes to receive a determination.
How far back do you have to file for medicaid?
It may take some time and effort to gather these documents, as some are required as far back as 5 years preceding the application date.
What is a Social Security letter?
Letter from the Social Security Administration that shows the amount of gross Social Security income & deductions the applicant receives. Income Verification Letter (s) or Tax Forms. Income verification letters or tax forms that document all income streams including: wages, pensions, royalties and / or interest.
Who can get medicaid?
In all states, Medicaid is available to low-income individuals and families, pregnant women, people with disabilities, and the elderly. Medicaid programs vary from state to state, and the Affordable Care Act (ACA) allows states to provide Medicaid to adults (under the age of 65) without minor children or a disability. 6 .
How much does Medicare pay for skilled nursing?
For the next 100 days, Medicare covers most of the charges, but patients must pay $176.00 per day (in 2020) unless they have a supplemental insurance policy. 3 .
How does Medicaid calculate the penalty?
Medicaid calculates the penalty by dividing the amount transferred by what Medicaid determines is the average price of nursing home care in your state. 12 . For example, suppose Medicaid determines your state's average nursing home costs $6,000 per month, and you had transferred assets worth $120,000.
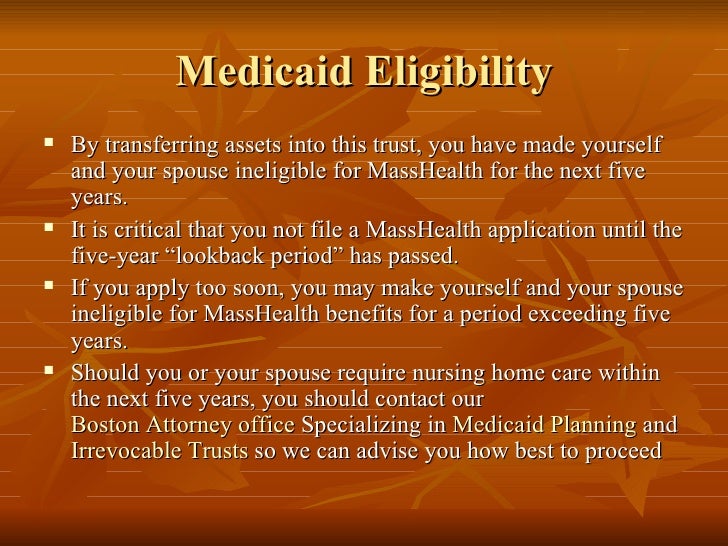
How long do you have to transfer assets to qualify for medicaid?
The transfer of assets must have occurred at least five years before applying to Medicaid in order to avoid ...
When was medicaid created?
Medicaid was created in 1965 as a social healthcare program to help people with low incomes receive medical attention. 1 Many seniors rely on Medicaid to pay for long-term nursing home care. “Most people pay out of their own pockets for long-term care until they become eligible for Medicaid.
What age can you transfer Medicaid?
Arrangements that are allowed include transfers to: 13 . Spouse of the applicant. A child under the age of 21. A child who is permanently disabled or blind. An adult child who has been living in the home and provided care to the patient for at least two years prior to the application for Medicaid.
Can you get Medicaid if you have a large estate?
Depending on Medicaid as your long-term care insurance can be risky if you have a sizeable estate. And even if you don't, it may not meet all your needs. But if you anticipate wanting to qualify, review your financial situation as soon as possible, and have an elder- or senior-care attorney set up your affairs in a way that will give you the money you need for now, while rendering your assets ineligible to count against you in the future.
Where are the requirements for Medicaid nursing facilities?
Specific requirements for Medicaid nursing facilities may be found primarily in law at section 1919 of the Social Security Act , in regulation primarily at 42 CFR 483 subpart B, and in formal Centers for Medicare & Medicaid Services guidance documents. Also see:
What are the requirements for nursing home?
Federal requirements specify that each NF must provide, (and residents may not be charged for), at least: 1 Nursing and related services 2 Specialized rehabilitative services (treatment and services required by residents with mental illness or intellectual disability, not provided or arranged for by the state) 3 Medically-related social services 4 Pharmaceutical services (with assurance of accurate acquiring, receiving, dispensing, and administering of drugs and biologicals) 5 Dietary services individualized to the needs of each resident 6 Professionally directed program of activities to meet the interests and needs for well being of each resident 7 Emergency dental services (and routine dental services to the extent covered under the state plan) 8 Room and bed maintenance services 9 Routine personal hygiene items and services
What is NF Medicaid?
A NF participating in Medicaid must provide, or arrange for, nursing or related services and specialized rehabilitative services to attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident.
What is long term care?
Long term care —health-related care and services (above the level of room and board) not available in the community, needed regularly due to a mental or physical condition. A nursing facility is one of many settings for long-term care, including or other services and supports outside of an institution, provided by Medicaid or other state agencies.
What is the definition of NF in Medicaid?
Specific to each state, the general or usual responsibilities of the NF are shaped by the definition of NF service in the state's Medicaid state plan, which may also specify certain types of limitations to each service. States may also devise levels of service or payment methodologies by acuity or specialization of the nursing facilities.
What services does a NF need?
Federal requirements specify that each NF must provide, (and residents may not be charged for), at least: Nursing and related services. Specialized rehabilitative services (treatment and services required by residents with mental illness or intellectual disability, not provided or arranged for by the state) Medically-related social services.
What is medically related social services?
Medically-related social services. Pharmaceutical services (with assurance of accurate acquiring, receiving, dispensing, and administering of drugs and biologicals) Dietary services individualized to the needs of each resident.
Does Medicaid Cover Nursing Home Care?
Learn about how Medicaid provides coverage for nursing home care, including eligibility rules and more. While Medicaid benefits vary from state to state, nursing home coverage is a mandatory Medicaid benefit.
Learn More About Medicare
Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage.
Table of Contents
What is Nursing Home Medicaid? Types of Medicaid that Cover Nursing Homes Medicaid Benefits in Nursing Homes Covered Services Service Not Covered How Income is Treated Beneficiary’s Income Spouse’s Income Understanding Family Supplementation Nursing Home Medicaid Eligibility Finding a Nursing Home that Takes Medicaid
What is Nursing Home Medicaid?
Designed for low-income Americans who need a high level of care because of age or chronic illness, Nursing Home Medicaid covers 100% of the costs of nursing home care. Nursing Home Medicaid is available in every state and is classified as an entitlement, which means anyone who is eligible (financially and medically) must be covered.
Types of Medicaid that Cover Nursing Homes
Nursing home Medicaid is also called Institutional Medicaid and is available for eligible Americans in every state. Nursing Home Medicaid is different from the other forms of Medicaid long term care, specifically Medicaid Waivers and Aged, Blind, and Disabled Medicaid (ABD is also called Regular Medicaid).
Medicaid Benefits in Nursing Homes
For those who are assessed as needing Medicaid (and who qualify financially), all costs including room and board are covered. What follows are the services that must be provided at nursing homes and covered under the Medicaid Long Term Care benefit.
What Happens to Income When They Enter a Nursing Home?
While Nursing Home Medicaid beneficiaries are permitted to earn a certain amount of income each month, all of that income (except for a very small personal needs allowance) must be surrendered to the nursing home in which they are receiving care.
Understanding Family Supplementation
It is possible for family members to give additional money to their loved one in a nursing home to pay for services not covered by Medicaid. However, it’s important to be careful about how “Family Supplementation” is offered, because receiving additional money can affect Medicaid eligibility.
Nursing Home Medicaid Eligibility
Eligibility requirements for Medicaid Long Term Care to cover nursing costs will vary by state and marital status. One can obtain their specific eligibility criteria here or read an article on Medicaid nursing home eligibility.
What is HCBS waiver?
HCBS Medicaid Waivers. Home and Community Based Services Medicaid wa ivers, also known as Section 1915 (c) waivers, are another way in which Medicaid offers in-home services and supports to promote independent living of elderly persons.
What are some examples of planning strategies?
There are also planning strategies, such as Miller Trusts, Medicaid asset protection trusts, irrevocable funeral trusts and annuities, that can be implemented in order for one to meet the financial eligibility criteria.
What are the eligibility requirements for Medicaid home care?
Eligibility Requirements for Medicaid Home Care. In order to be eligible for Medicaid, and hence, in-home care, there are eligibility requirements that must be met. In addition to being a resident in the state in which one applies, there are also financial and functional needs that must be met.
How much income can I have on Medicaid in 2021?
As a general rule of thumb, in 2021, 300% of SSI is used as the income limit. This means that an individual cannot have more than $2,382 / month in income. There is also an asset limit, which in most cases, is $2,000.
What is HCBS section 1915?
The section 1915 (i) HCBS state plan option allows persons to receive in-home care assistance, including skilled nursing services, respite care, and home modifications. With this option, persons are not required to demonstrate a need for a nursing home level of care.
What is regular state medicaid?
With regular state Medicaid, also referred to as original Medicaid and classic Medicaid, the federal government requires that states make home health benefits available to those in need.
What is a CFC in healthcare?
One such alternative, made possible by the Affordable Care Act, is the Community First Choice (CFC) option. CFC allows states to offer in-home personal attendant services to assist with one’s activities of daily living (ADLs) ...
How to apply for medicaid online?
Create & Submit Application 1 Apply online#N#Visit www.gateway.ga.gov. Select Apply for Benefits to begin.#N#Select Medical Assistance as a program.#N#Follow the online prompts to apply for Medicaid. 2 Apply by phone#N#You can apply by phone by calling 877-423-4746.#N#After your call, you may need to provide additional information or documentation. 3 Apply in person#N#You can apply in person through your county Division of Family and Children Services (DFCS) office.#N#Be sure to bring all required documentation for your visit. 4 Apply by mail#N#You can apply by mail by calling 877-423-4746 and requesting to have forms mailed to you.#N#Complete all forms mailed to you as directed and mail back to the Division of Family and Children Services.#N#You may need to provide additional information or documentation.
What happens when you complete a medicaid application?
Once you complete an application for Medicaid, an eligibility specialist will review your application. The eligibility specialist will make sure all necessary information has been received. A Medicaid caseworker will interview you and review your application.
How long does it take to get a medicaid card?
You will find out by mail whether you are eligible for Medicaid within 45 days after you apply. (If you have a disability and it has to be determined, the process may take up to 60 days). If you are eligible for Medicaid, you will receive a Medicaid card in the mail.
What happens if you are ineligible for medicaid based on income?
If you are ineligible for Medicaid based on income, your information will be transferred to the Federally Facilitated Marketplace (FFM) to determine if you qualify for subsidies, cost-sharing reductions, premium tax credits, or private health coverage.
How long does it take to get a medicaid test?
A free, non-binding Medicaid eligibility test is available here. This test takes approximately 3 minutes to complete. Readers should be aware the maximum income limits change dependent on the marital status of the applicant, whether a spouse is also applying for Medicaid and the type of Medicaid for which they are applying.
What are the expenses that go away when you receive Medicaid at home?
When persons receive Medicaid services at home or “in the community” meaning not in a nursing home through a Medicaid waiver, they still have expenses that must be paid. Rent, mortgages, food and utilities are all expenses that go away when one is in a nursing home but persist when one receives Medicaid at home.
Is income the only eligibility factor for Medicaid?
Medicaid Eligibility Income Chart by State – Updated Mar. 2021. The table below shows Medicaid’s monthly income limits by state for seniors. However, income is not the only eligibility factor for Medicaid long term care, there are asset limits and level of care requirements.
