Predetermination of Benefits are:
- Voluntary utilization management reviews
- Not necessary for services and drugs on the prior authorization list
- May be used if you are not sure about coverage or whether we may not consider it medically necessary
How is the predetermination of benefits determined?
The predetermination of benefits depends on information your doctor sends to Blue Cross and Blue Shield of Texas (BCBSTX) medical staff. You may think, “If my doctor tells me I need something, why does it need a second approval?
What is predetermination of benefits for dental insurance?
Predetermination of benefits for Dental Insurance: What is it? It’s a statement from the insurance company stating what they’ll pay towards the procedures you sent in on the Predetermination claim.
What is a predetermination of benefits from AHA?
A predetermination of benefits is a review by your insurer’s medical staff. They decide if they agree that the treatment is right for your health needs. Predeterminations are done before you get care, so you will know early if it is covered by your health insurance plan.
What is a predetermination payment statement?
It’s a statement from the insurance company stating what they’ll pay towards the procedures you sent in on the Predetermination claim.

What is the difference between a predetermination and a prior authorization?
Benefit coverage is predetermined before services are rendered and any limitation under a plan can be addressed before services are rendered. A predetermination is a courtesy, where a pre-authorization is a requirement under a plan.
What does a predetermination mean?
Definition of predetermination 1 : the act of predetermining : the state of being predetermined: such as. a : the ordaining of events beforehand. b : a fixing or settling in advance.
What is a predetermination request?
A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient's health benefit plan. Predetermination approvals and denials are based on our medical policies, coverage documents and benefits. View Medical Coverage Policies.
What is a predetermination letter for insurance?
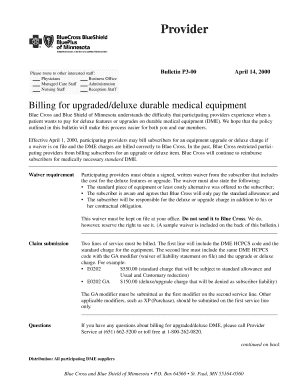
Pre-determination letters are submitted on the provider's letterhead. The letter requests advance verification that the patient is covered for the medical service. Failure to submit a pre-certification letter usually results in denial of the claim for payment.
What is an example of predetermination?
A secular example to try to illustrate predeterminism is that a fetus's future physical, emotional, and other personal characteristics as a matured human being may be considered "predetermined" by heredity, i.e. derived from a chain of events going back long before her eventual birth.
What is a predetermination of dental benefits?
Feb 28, 2020. A predetermination of benefits is a written estimate from your dental insurer of the amount your dental plan will pay for a specific treatment based on information provided by your dentist. SDC's predetermination process is helpful for both the patient and the treating dentist.
What is prior authorization in medical billing?
In the medical billing world, preauthorization, prior authorization, precertification, and notification are terms that may be used interchangeably to mean that for certain situations and procedures, providers have to contact insurers in advance and obtain a certification number in order to be reimbursed properly (or at ...
What is pre certification in healthcare?
A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment is medically necessary. Sometimes called prior authorization, prior approval or precertification.
What is a post service review?
What is post-payment service-specific review? A. A post-payment review is conducted on services/claims that have already been submitted and paid by Medicare to the provider. First Coast is required to review documentation that substantiates information reported on claims submitted for reimbursement.
Under what circumstances is it the patient's responsibility to obtain pre authorization approval?
Prior Authorizations Under medical and prescription drug plans, some treatments and medications may need approval from your health insurance carrier before you receive care. Prior authorization is usually required if you need a complex treatment or prescription. Coverage will not happen without it.
What is the purpose of the assignment of benefits?
Assignment of Benefits (AOB) is an agreement that transfers the insurance claims rights or benefits of the policy to a third-party. An AOB gives the third-party authority to file a claim, make repair decisions, and collect insurance payments without the involvement of the homeowner.
What does coordination of benefits allow?
Coordination of benefits (COB) allows plans that provide health and/or prescription coverage for a person with Medicare to determine their respective payment responsibilities (i.e., determine which insurance plan has the primary payment responsibility and the extent to which the other plans will contribute when an ...
What is predetermination for health insurance?
Predetermination for benefits of your health insurance plan is a process through which your insurer’s medical staff reviews the recommended treatment. If they agree with your doctors and specialists that you need the health treatment and that it is right for you, your predetermination is approved. They are typically done before you receive care, ...
What is the predetermination requirement for life threatening conditions?
Anything not deemed life threatening typically falls under the predetermination requirement. Providers must submit the predetermination letter using their letterhead. If they fail to send a letter in with the request for coverage, the claim is likely to be denied.
How long does it take for a predetermination to be approved?
This predetermination gives you a peace of mind regardless of the treatment you’ve applied for. However, these requests can also take up to forty-five days for approval.
How long does it take to get a preauthorization?
Regardless, failing to get preauthorization could cause a non-reimbursement for your treatment. Keep in mind that this process can take up to thirty days to be approved. Pay special attention to your preauthorization number on the document to ensure that that your claim is accurately submitted and reported back to you.
Is the bottom line important in insurance?
When your health is at stake, nothing is more important than getting the best care possible. That is what your insurer is trying to help you do, in most instances. Yet, the bottom line does play a role in approval rates.
Is predetermination good for you?
But you might still be wondering why predetermination is good for you. After all, it generally seems like more of a hassle than it is worth. However, as healthcare consultants, we know there are multiple benefits of predetermination for both you and for your insurer.
What is a dental predetermination?
A predetermination of benefits is a written estimate from your dental insurer of the amount your dental plan will pay for a specific treatment based on information provided by your dentist.
Can a dentist submit a predetermination to SDC?
Since documentation requirements are satisfied before treatment begins, predeterminations can also expedite claim payment. You can ask your dentist to submit a predetermination of benefits to SDC for any treatment or service before it is performed.
What is Delta Dental Predetermination?
A Delta Dental predetermination of benefits is most often requested for costly procedures such as crowns, wisdom tooth extractions, bridges, implants, dentures, and oral surgery.
Is predetermination of benefits a guarantee?
The predetermination of benefits that we provide is just an estimate. It is not a guarantee, but rather our best estimation of the costs for which you will be responsible. If your benefits change before the treatment is completed (or starts), the estimate won’t be accurate.
What does it mean when a predetermination for implant placement comes back as approved?
For example: if a Predetermination for implant placement comes back as approved with 60% coverage and $800 of estimated insurance coverage – it means as long as the patient has $800 left in their plan at time you submit the claim after placing the implant – the benefit will be paid at the rate listed in the pre-estimate.
Do all plans require predetermination?
Not all plans require Predetermination to be done, but for the ones that do for any specific procedure, I’ve followed a routine to have all the information during treatment planning visit. Procedure. Recommended X-rays and Documentation. Root Canal.
Is a predetermination statement a guarantee of payment?
What they’re saying is, the Predetermination statement is NOT a guarantee of payment.
How long does it take to get a predetermination EOB?
It’s important to know because if a plan REQUIRES a predetermination to be sent for a procedure, and the date on the predetermination EOB is more than 90 days, then you risk getting the procedure denied when you submit the actual CLAIM along with the predetermination.
What is an EOB code?
EOB Code: These are short codes for explaining why a procedure is getting denied, or downgraded. You may find one of more codes on a line item or procedure. Towards the bottom – you see the explanation of K16 – according to this EOB, United Health care doesn’t seem this crown is necessary for this patient.
Why is there zero on EOB?
It’s zero on this EOB because the procedure is denied. Again, this may show up differently for another plan. This sometimes is referred to as “negotiated amount” on other plans’ EOB statements. Patient responsibility: this is the patient portion of payment required for the procedure.
Does insurance approve predetermination?
After you send in the predetermination along with all the supported documentation, the insurance may approve the procedures you’re requesting for the patient or they may deny one or more of those procedures.
What is a predetermination letter?
A "pre-determination letter" is part of the claims management process for health insurance providers. The letter relates to the coverage of specific medical services under a patient's policy. Insurance companies require health care providers to follow submission instructions, such as the content that must be included in the pre-determination letter.
What is pre-certification in insurance?
Pre-certification is required for hospital admission and surgical procedures. Pre-authorization and pre-certification confirm medical necessity before the insurer approves or pays a claim. Pre-determination confirms that the patient’s policy covers ...
What happens if you don't submit a pre-certification letter?
Failure to submit a pre-certification letter usually results in denial of the claim for payment. The American Medical Association recommends that physicians also submit pre-determination letters for services and procedures that an insurer frequently denies as medically unnecessary.